Rapid Diagnostic Tests For Gonorrhea
Gonorrhea is a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae. It is one of the most common sexually transmitted infections worldwide, affecting millions of people each year. Early detection and prompt treatment of gonorrhea are crucial to prevent the spread of the infection and its complications.
Traditional diagnostic methods for gonorrhea
In the past, diagnosing gonorrhea relied on time-consuming and complex laboratory techniques, such as culture and nucleic acid amplification tests (NAAT). Culture involves growing the bacteria in a laboratory setting, which can take up to several days to produce results. NAAT, while more sensitive and specific, also requires specialized laboratory equipment and skilled personnel.
The advent of rapid diagnostic tests
In recent years, there has been a significant development in rapid diagnostic tests for gonorrhea. These tests offer quick and accurate results, allowing for timely treatment and reducing the risk of further transmission.
Types of rapid diagnostic tests
There are various types of rapid diagnostic tests available for gonorrhea. Some of these tests detect the presence of gonococcal antigens, while others detect the bacterium’s genetic material, such as DNA or RNA. These tests can be performed on different types of specimens, including urine, vaginal swabs, and urethral samples.
Benefits of rapid diagnostic tests
Rapid diagnostic tests for gonorrhea offer several advantages. Firstly, they provide results within minutes to hours, enabling healthcare providers to diagnose and treat patients on the same visit. This reduces the chances of patients being lost to follow-up and ensures prompt management of the infection.
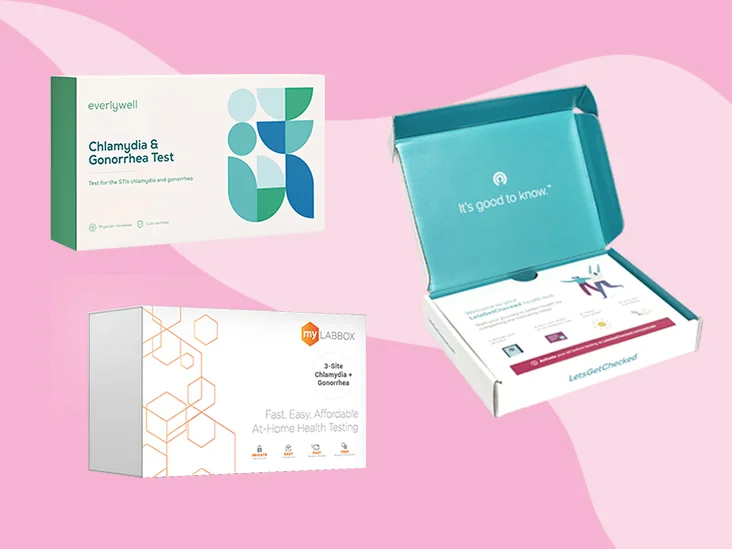
Secondly, rapid diagnostic tests can be performed in various healthcare settings, including point-of-care facilities, community clinics, and even home testing kits. This accessibility allows for widespread screening and early detection of gonorrhea, reaching populations that may have limited access to traditional laboratory-based tests.
rapid diagnostic tests have shown comparable sensitivity and specificity to traditional laboratory methods. This means that they provide accurate results, allowing for reliable diagnosis and appropriate treatment.
rapid diagnostic tests for gonorrhea have revolutionized the diagnosis and management of this sexually transmitted infection. Their speed, ease of use, and accuracy make them valuable tools for healthcare providers in combating the spread of gonorrhea and its associated complications.
Point-Of-Care Gonorrhea Testing
Gonorrhea is a sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae. It is one of the most common bacterial STIs worldwide, with millions of new cases reported each year. Early and accurate diagnosis of gonorrhea is crucial for effective treatment and prevention of complications. One approach to improving the accessibility and efficiency of gonorrhea testing is through point-of-care (POC) testing.
Point-of-care testing refers to diagnostic tests that can be performed at the patient’s side, without the need for samples to be sent to a laboratory for analysis. These tests provide rapid results, often within minutes, enabling healthcare providers to make immediate treatment decisions. POC testing for gonorrhea offers several advantages over traditional laboratory-based testing methods.
Firstly, POC testing eliminates the need for sample transportation and laboratory processing, reducing the turnaround time for results. This is particularly beneficial in low-resource settings or areas with limited access to laboratory facilities. Patients can receive their test results promptly, and if necessary, start treatment immediately, reducing the risk of transmission and potential complications.
- Secondly, POC tests are typically simple to use, requiring minimal training and expertise to perform. This makes them suitable for use in various healthcare settings, such as primary care clinics, emergency departments, or even non-traditional settings like community outreach programs. By enabling testing to be conducted closer to the point of patient care, POC testing helps improve overall healthcare delivery and patient outcomes.
- POC tests for gonorrhea are highly sensitive and specific, providing accurate results comparable to laboratory-based tests. Advances in technology have allowed for the development of rapid diagnostic tests that detect specific antigens or genetic material of the Neisseria gonorrhoeae bacterium. These tests often utilize immunoassays or nucleic acid amplification techniques, ensuring accurate detection of the infection.
| Advantages of Point-of-Care Gonorrhea Testing: |
|---|
| Rapid Results: Immediate access to test results. |
| Increased Accessibility: Testing can be performed in a variety of healthcare settings. |
| Accuracy: Highly sensitive and specific tests are available. |
point-of-care gonorrhea testing offers a convenient and effective approach to diagnosing and managing this prevalent STI. Its rapid results, increased accessibility, and accuracy make it a valuable tool in combating the spread of gonorrhea and its associated complications. As further advancements are made in the field of POC testing, it is anticipated that these tests will continue to play a vital role in the early detection and control of gonorrhea.
Advancements In Nucleic Acid Amplification Tests
Nucleic acid amplification tests (NAATs) have revolutionized the field of diagnostics by providing highly sensitive and specific detection of various pathogens, including gonorrhea. These tests have become an indispensable tool in the diagnosis and management of infectious diseases, allowing for early detection and treatment. Over the years, there have been significant advancements in NAATs, which have further improved their accuracy and expanded their utility in the field of gonorrhea testing.
One of the key advancements in nucleic acid amplification tests is the development of real-time polymerase chain reaction (PCR) technology. This technique allows for the rapid and simultaneous amplification and detection of specific nucleic acid sequences of the gonorrhea-causing bacteria, Neisseria gonorrhoeae. Real-time PCR offers several advantages over traditional PCR, including shorter turnaround times, higher sensitivity, and the ability to quantify the amount of bacteria present in a sample.
Another significant advancement in NAATs is the introduction of isothermal amplification methods, such as loop-mediated isothermal amplification (LAMP) and helicase-dependent amplification (HDA). These techniques eliminate the need for thermal cycling, making them more suitable for point-of-care testing and resource-limited settings. LAMP and HDA assays have shown excellent sensitivity and specificity for gonorrhea diagnosis, making them valuable tools in the fight against this sexually transmitted infection.
- advancements in nucleic acid amplification tests have greatly improved the accuracy and utility of gonorrhea testing. Real-time PCR and isothermal amplification methods, such as LAMP and HDA, have revolutionized the field by providing rapid, sensitive, and specific detection of Neisseria gonorrhoeae. These tests have transformed the diagnosis and management of gonorrhea, allowing for early detection, appropriate treatment, and prevention of further spread of the infection. As technology continues to advance, we can expect further enhancements in the sensitivity, specificity, and ease of use of nucleic acid amplification tests, ultimately leading to better patient outcomes.
| Advancements In Nucleic Acid Amplification Tests |
|---|
| – Real-time polymerase chain reaction (PCR) technology |
| – Loop-mediated isothermal amplification (LAMP) and helicase-dependent amplification (HDA) |
| – Improved accuracy and utility in gonorrhea testing |
Improved Accuracy With Molecular Diagnostics
Molecular diagnostics is a rapidly advancing field in healthcare, offering improved accuracy and precision in disease diagnosis. This technology is particularly valuable in the case of gonorrhea, a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae. Traditionally, the diagnosis of gonorrhea has relied on culture-based methods, which can be time-consuming and may yield false-negative results. However, with the advent of molecular diagnostics, healthcare providers now have access to highly sensitive and specific tests that can detect the presence of N. gonorrhoeae DNA in patient samples.
Molecular diagnostics for gonorrhea utilizes the amplification of nucleic acids, such as DNA or RNA, to detect the genetic material of the infecting organism. This approach offers several advantages over traditional culture methods, including enhanced sensitivity, faster turnaround time, and the ability to detect multiple strains or antibiotic-resistant variants of N. gonorrhoeae. Molecular tests rely on various techniques, such as polymerase chain reaction (PCR), nucleic acid hybridization, and sequence-specific oligonucleotide probes, to identify the presence of the bacteria.
One of the key benefits of molecular diagnostics is its ability to detect low levels of bacterial DNA, even in the early stages of infection. This can significantly improve the accuracy of diagnosis, especially in cases where the bacterial load is low or when asymptomatic individuals are being tested. molecular tests offer greater specificity by targeting specific regions of the bacterial genome, minimizing the risk of false-positive results. This ensures that patients receive appropriate treatment and reduces the likelihood of unnecessary antibiotic use.
- The advantages of molecular diagnostics in gonorrhea testing can be summarized as:
| Improved Accuracy | Enhanced Sensitivity | Specificity |
|---|---|---|
| Molecular diagnostics provide highly accurate results compared to traditional culture methods, reducing the likelihood of false-negative or false-positive results. | The sensitivity of molecular tests allows for the detection of low levels of bacterial DNA, improving the ability to diagnose gonorrhea in its early stages. | By targeting specific regions of the bacterial genome, molecular tests offer enhanced specificity, minimizing the risk of false-positive results and unnecessary treatment. |
molecular diagnostics have revolutionized the field of gonorrhea diagnosis, offering improved accuracy, sensitivity, and specificity compared to traditional methods. These advancements enable healthcare providers to detect the presence of N. gonorrhoeae with greater precision, ensuring timely and appropriate treatment for patients. As technology continues to evolve, molecular diagnostics will continue to play a crucial role in the fight against gonorrhea and other infectious diseases.
Next-Generation Sequencing For Gonorrhea Diagnosis
Next-generation sequencing (NGS) has revolutionized the field of genomics, allowing for faster and more accurate sequencing of DNA and RNA. This technology has also found its application in the diagnosis of infectious diseases, including gonorrhea. Gonorrhea is a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae. Traditionally, diagnosis of gonorrhea relied on culture-based methods, which were time-consuming and often lacked sensitivity. However, with the advent of NGS, there has been a significant improvement in the diagnosis of gonorrhea, enabling rapid and comprehensive detection of the causative agent.
One of the major advantages of using NGS for gonorrhea diagnosis is its ability to simultaneously sequence multiple samples in a single run. This high-throughput capacity allows for the detection of various strains and genetic variations within the bacterial population, providing valuable insights into the epidemiology and drug resistance patterns of gonorrhea. By analyzing the entire genome of the pathogen, NGS can identify specific genetic markers associated with antibiotic resistance, helping in the selection of appropriate treatment options. This approach has the potential to greatly enhance the control and management of gonorrhea, especially in the face of increasing antibiotic resistance.
In addition to its advantages in terms of speed and sensitivity, NGS also offers the ability to detect co-infections or mixed infections with other pathogens. This is particularly relevant in the context of sexually transmitted infections, where individuals may be infected with multiple pathogens simultaneously. By sequencing the entire microbial community present in a sample, NGS can identify other potential pathogens that may be present alongside N. gonorrhoeae. This comprehensive approach to diagnosis can aid in the identification of co-infections and facilitate appropriate treatment strategies.
- Improved accuracy: NGS provides a higher level of accuracy compared to traditional culture-based methods, reducing the chances of false negative or false positive results.
- Comprehensive analysis: The ability to analyze the entire genome allows for the detection of genetic variations and antibiotic resistance markers, providing a more complete picture of the infection.
- Identification of co-infections: NGS can detect other potential pathogens present in a sample, enabling the identification of co-infections and guiding appropriate treatment.
| Advantages | Disadvantages |
|---|---|
| High accuracy | Costly |
| Comprehensive analysis | Technical expertise required |
| Identification of co-infections | Turnaround time |
Emerging Technologies For Detecting Antibiotic Resistance
With the increasing rate of antibiotic resistance, it is essential to develop innovative technologies for the detection of antibiotic resistance in pathogens. Emerging technologies have provided new avenues for identifying and monitoring antibiotic resistance, enabling timely and effective treatment strategies. These technologies offer quicker and more accurate results, allowing healthcare professionals to make informed decisions about the choice and dosage of antibiotics.
One such emerging technology is **molecular diagnostics**, which involves the detection of specific genes or genetic mutations associated with antibiotic resistance. This technique relies on nucleic acid amplification tests (NAATs) to amplify and detect the target genes. NAATs offer exceptional sensitivity and specificity, enabling the identification of resistant strains even at low concentrations. they can simultaneously detect multiple resistance genes, providing a comprehensive understanding of the resistance profile.
Another promising technology for detecting antibiotic resistance is **next-generation sequencing (NGS)**. NGS allows for the rapid and high-throughput sequencing of entire genomes or specific genes, providing a detailed understanding of the genetic basis of resistance. By sequencing the genes involved in antibiotic resistance, healthcare professionals can accurately identify the resistance mechanisms and predict the effectiveness of different antibiotics. This information can guide the selection of appropriate antibiotics, improving patient outcomes.
Promising Biomarkers In Gonorrhea Diagnosis
Gonorrhea is a common sexually transmitted infection (STI) that can have serious health consequences if left untreated. Early and accurate diagnosis is essential for effective management and control of the disease. Traditional diagnostic methods for gonorrhea involve culturing the bacteria and identifying it under a microscope. However, these methods are time-consuming and may not always yield accurate results. In recent years, there have been significant advancements in diagnostic techniques, particularly in the identification of promising biomarkers for gonorrhea diagnosis.
One such promising biomarker is the nucleic acid amplification test (NAAT), which detects the genetic material (DNA or RNA) of the gonorrhea-causing bacteria. NAATs offer high sensitivity and specificity, making them a reliable tool for diagnosing gonorrhea. These tests can be performed on various specimens, including urine, vaginal swabs, and rectal swabs. The use of NAATs has greatly improved the accuracy of gonorrhea diagnostics, allowing for earlier detection and timely treatment.
Another promising biomarker for gonorrhea diagnosis is the detection of specific antigens or proteins produced by the bacteria. These biomarkers can be identified using immunoassays, such as enzyme-linked immunosorbent assays (ELISAs) or lateral flow assays (LFAs). These tests are rapid, easy to use, and can be performed at the point of care, eliminating the need for laboratory infrastructure. Point-of-care testing for gonorrhea not only improves patient outcomes but also aids in the prevention of further transmission of the infection.
- Advancements in diagnostic techniques have also led to the exploration of next-generation sequencing (NGS) for gonorrhea diagnosis. NGS allows for the rapid and comprehensive analysis of the genetic material of the bacteria, providing valuable insight into drug resistance and epidemiological patterns. This information can help inform treatment decisions and guide public health interventions.
- Emerging technologies, such as microfluidic devices and miniaturized biosensors, hold promise in the detection of antibiotic resistance in gonorrhea. These technologies enable rapid and sensitive detection of specific genetic markers associated with resistance to commonly used antibiotics. Early identification of antibiotic-resistant strains is crucial for appropriate treatment selection and effective disease management.
- Furthermore, advancements in urine-based gonorrhea testing have revolutionized the diagnostic process. Urine samples are easy to collect and non-invasive, making them ideal for large-scale screening programs. The development of sensitive and specific urine-based tests has greatly enhanced the accessibility and accuracy of gonorrhea diagnosis.
| Advantages ofNon-Invasive Gonorrhea Diagnosis: | Enhancing Sensitivity andSpecificity of Gonorrhea Tests: |
|---|---|
| 1. Easy sample collection. | 1. Utilization of promising biomarkers. |
| 2. High patient acceptance and convenience. | 2. Improved accuracy and reliability. |
| 3. Suitable for large-scale screening. | 3. Early detection of infection. |
the identification and utilization of promising biomarkers in gonorrhea diagnosis have revolutionized the field of STI diagnostics. These biomarkers, including those detected through NAATs, antigen detection assays, and next-generation sequencing, offer improved accuracy, rapid results, and ease of use. non-invasive testing methods, such as urine-based tests, provide convenience and accessibility for both patients and healthcare providers. These advancements not only aid in early detection and treatment but also contribute to the effective control and prevention of gonorrhea.
Innovations In Urine-Based Gonorrhea Testing
Gonorrhea is a sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae. It is one of the most common STIs globally, with millions of new cases reported each year. Timely and accurate diagnosis of gonorrhea is crucial for effective treatment and prevention of further transmission. In recent years, there have been significant innovations in the field of urine-based gonorrhea testing, offering several advantages over traditional diagnostic methods.
One notable innovation is the development of nucleic acid amplification tests (NAATs) for urine-based gonorrhea testing. NAATs are highly sensitive and specific, allowing for the detection of even low levels of the N. gonorrhoeae bacteria in urine samples. This eliminates the need for invasive and uncomfortable specimen collection methods, such as urethral or cervical swabs, making urine-based testing more convenient and acceptable for patients.
Another innovation in urine-based gonorrhea testing is the incorporation of point-of-care (POC) technologies. POC tests enable rapid detection of gonorrhea in resource-limited settings, such as primary care clinics or community health centers. These tests provide results within minutes, allowing for immediate diagnosis and initiation of treatment, thereby reducing the risk of complications and further transmission. POC tests often require minimal laboratory infrastructure and technical expertise, making them suitable for use in a variety of healthcare settings.
- Advancements in urine-based gonorrhea testing have also focused on improving the accuracy of diagnostic methods. Molecular diagnostic techniques, such as polymerase chain reaction (PCR), have been used to enhance the sensitivity and specificity of gonorrhea tests. PCR-based tests target specific regions of the N. gonorrhoeae genome, enabling highly precise and reliable detection of the bacteria in urine samples. These advancements in accuracy are crucial for effective diagnosis and appropriate management of gonorrhea.
| Advantages of Urine-Based Gonorrhea Testing |
|---|
| The use of urine samples for gonorrhea testing has several advantages: |
| Non-invasive: Urine samples can be easily collected without the need for invasive procedures, such as swabs or blood tests. This makes urine-based testing more convenient and acceptable for patients, resulting in increased testing rates and early detection of gonorrhea. |
| Accessibility: Urine-based testing can be performed in a variety of healthcare settings, including primary care clinics, community health centers, and even at home. This improves access to testing, particularly for individuals who may face barriers to seeking healthcare services. |
| High sensitivity and specificity: The advancements in urine-based gonorrhea testing techniques, such as NAATs and PCR, have significantly improved the accuracy of diagnosis. These tests can detect very low levels of N. gonorrhoeae bacteria, ensuring reliable results and appropriate management of the infection. |
innovations in urine-based gonorrhea testing have revolutionized the diagnosis and management of this common STI. The use of NAATs, POC technologies, and molecular diagnostic methods has greatly enhanced the accuracy, convenience, and accessibility of gonorrhea testing, leading to early detection and appropriate treatment. These advancements are crucial in the global efforts to control and prevent the spread of gonorrhea, highlighting the importance of continued research and development in this field.
Advantages Of Non-Invasive Gonorrhea Diagnosis
Gonorrhea is a sexually transmitted infection that affects millions of people worldwide. Traditionally, the diagnosis of gonorrhea has relied on invasive methods such as swabbing the infected area for culture testing. However, advancements in medical technology have led to the development of non-invasive diagnostic methods that offer several advantages. In this blog post, we will explore the advantages of non-invasive gonorrhea diagnosis and how these methods are revolutionizing the field of sexual health.
1. Less discomfort: One of the primary advantages of non-invasive gonorrhea diagnosis is that it is far less uncomfortable for patients. Unlike invasive methods, which involve swabs or biopsies, non-invasive tests can be performed using urine samples or blood tests. This eliminates the need for physical discomfort and makes it easier for individuals to undergo testing.
2. Greater accessibility: Non-invasive gonorrhea diagnosis methods are more accessible to a wider range of individuals. Invasive procedures may require specialized medical equipment and trained personnel, which may not be available in all healthcare settings. Non-invasive tests, on the other hand, can be easily administered in various healthcare settings, including clinics and community health centers, making them more widely available to the general public.
3. Increased patient compliance: Non-invasive gonorrhea diagnosis methods also have the potential to increase patient compliance with testing. For individuals who may be reluctant or hesitant to undergo invasive procedures, non-invasive tests offer a more appealing option. This can lead to higher rates of testing, earlier detection of infections, and better overall management of gonorrhea in the population.
- Conclusion:non-invasive gonorrhea diagnosis methods present several advantages over traditional invasive procedures. These tests offer less discomfort for patients, greater accessibility in healthcare settings, and increased patient compliance. As the field of sexual health continues to evolve, these advancements in non-invasive testing will play a crucial role in the early detection and management of gonorrhea infections. It is important for healthcare professionals and policymakers to continue to explore and invest in these innovative diagnostic methods to effectively combat the global burden of gonorrhea.
| Advantages of Non-Invasive Gonorrhea Diagnosis |
|---|
| Less discomfort |
| Greater accessibility |
| Increased patient compliance |
Enhancing Sensitivity And Specificity Of Gonorrhea Tests
Gonorrhea is a common sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae. It can affect both men and women and often presents with symptoms such as pain or burning during urination, genital discharge, and genital itching. Early detection and accurate diagnosis of gonorrhea are crucial for effective treatment and prevention of its spread. In recent years, there have been significant advancements in the field of diagnostic testing for gonorrhea, specifically in enhancing the sensitivity and specificity of these tests.
Rapid diagnostic tests for gonorrhea: Rapid diagnostic tests (RDTs) have emerged as a valuable tool in the diagnosis of gonorrhea. These tests are designed to provide quick results, usually within 30 minutes, allowing for immediate initiation of treatment if necessary. RDTs for gonorrhea detect the presence of specific antigens or genetic material associated with N. gonorrhoeae in a patient’s urine, blood, or genital swab samples. They offer high sensitivity and specificity, enabling accurate diagnosis even in asymptomatic individuals.
Point-of-care gonorrhea testing: Point-of-care (POC) testing has revolutionized the field of diagnostics, allowing for rapid and accurate diagnosis at the patient’s bedside or in non-laboratory settings. POC gonorrhea tests can be performed using handheld devices or portable diagnostic platforms, providing results within minutes. These tests often utilize nucleic acid amplification techniques to detect the presence of N. gonorrhoeae. POC testing not only enhances sensitivity and specificity but also enables timely and targeted treatment, reducing the risk of complications and transmission.
Frequently Asked Questions
What is the benefit of using rapid diagnostic tests for gonorrhea?
Rapid diagnostic tests for gonorrhea are advantageous because they provide quick results, allowing for immediate initiation of treatment and prevention of further transmission of the infection.
What is point-of-care gonorrhea testing?
Point-of-care gonorrhea testing refers to testing that can be performed at the point of care, such as a healthcare clinic or doctor’s office, without the need for laboratory facilities. This enables faster diagnosis and treatment decisions.
How have nucleic acid amplification tests advanced gonorrhea testing?
Nucleic acid amplification tests have revolutionized gonorrhea testing by detecting the genetic material of the bacteria, offering high sensitivity and specificity even in cases with low bacterial loads. They have improved the accuracy of diagnosis.
What is the role of molecular diagnostics in improving accuracy of gonorrhea testing?
Molecular diagnostics, such as polymerase chain reaction (PCR) and DNA sequencing, have enhanced the accuracy of gonorrhea testing by directly detecting the DNA or RNA of the bacteria. This eliminates the possibility of false positives or negatives.
How can next-generation sequencing contribute to gonorrhea diagnosis?
Next-generation sequencing technologies enable the rapid and comprehensive analysis of the entire genetic material of the gonorrhea bacteria. This can help identify drug resistance and genetic variations, aiding in targeted treatment strategies.
What emerging technologies are being developed to detect antibiotic resistance in gonorrhea?
Emerging technologies, such as whole-genome sequencing and loop-mediated isothermal amplification (LAMP), are being explored for their ability to detect antibiotic resistance in gonorrhea. These methods can help guide appropriate antibiotic choices for effective treatment.
Are there any promising biomarkers for gonorrhea diagnosis?
Promising biomarkers, such as specific proteins or genetic markers, are being investigated for their potential role in the diagnosis of gonorrhea. These biomarkers could contribute to more accurate and efficient diagnosis in the future.
What are the advantages of urine-based gonorrhea testing?
Urine-based gonorrhea testing offers several advantages, including non-invasive sample collection, ease of testing, and the ability to detect gonorrhea infections in both males and females. It eliminates the need for uncomfortable swab collection methods.
How can sensitivity and specificity of gonorrhea tests be enhanced?
The sensitivity and specificity of gonorrhea tests can be enhanced through technological improvements, validation studies, and continuous quality assurance. Ongoing research and development aim to optimize these tests for better accuracy in diagnosing gonorrhea.